Today in Part 10 of my global series, "Ticks", I am joined by three of these pioneers: Dr. Brian Fallon, Dr. Judith Miklossy and Dr. Eva Sapi. Dr. Sapi is Associate Professor at the University of New Haven (CT) where she carries out Lyme disease research with her graduate students. To date, over 70 graduate students have received training in Lyme disease related research. Dr. Judith Miklossy is Director of the Alzheimer Research Center in Switzerland. She is an expert in spirochete microbiology and neuropathology. Dr. Miklossy serves on the boards of several international Lyme disease foundations. Dr. Brian Fallon is Professor of Clinical Psychiatry and Director of the Lyme and Tick-borne Diseases Research Center at Columbia University Medical Center.
Brian, would you please summarize for me what you think tick-borne disease research has accomplished in the last five years?
There have been major advances. We've learned from the animal models that the Lyme infection can persist in small numbers despite antibiotic treatment; this has long been suspected by clinicians working with humans - having it demonstrated in several animal models allows us to investigate whether these persistent organisms in the animals are causing disease. We've learned from studies of patients with chronic symptoms after treatment for Lyme disease that the immune system is often hyper-activated -- that patients have elevated immune activity in the blood and in their spinal fluid. This overactive immune system itself may be leading to the chronic symptoms of fatigue, pain, and cognitive dysfunction. We've learned from studies of ticks that about 30% carry more than one pathogen and that the new microbe, Borrelia miyamotoi, can cause a Lyme-like illness that responds to antibiotics but which will not test positive on Lyme testing. This may explain why some patients with a Lyme-like illness never tested positive for Lyme but did get better after antibiotic therapy.
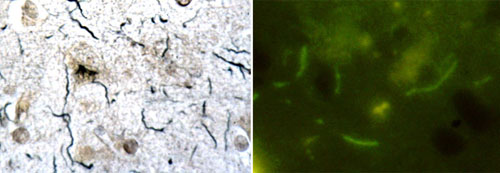
Eva: Our research group studies different forms of Borrelia bacteria to better understand how Borrelia can hide from the immune system and from different therapies. For example, our research group demonstrated that Borrelia is capable of forming a protective layer around itself - called biofilm - which could render it to be very resistant to antibiotics and provide a logical explanation as to why extensive antibiotic treatment for patients with a tick-bite history could fail. Our final goal is to better understand Borrelia survival mechanisms, and ultimately to provide new research information for the chronic Lyme debate. Previously, our Lyme disease research group has also identified an alarming increase in the co-infection rate in deer ticks, including discovery of novel co-infections such as mycoplasma and microfilarial nematode species.
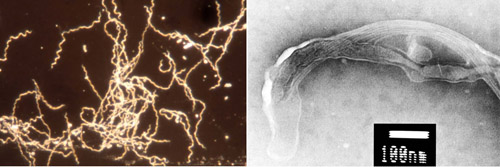
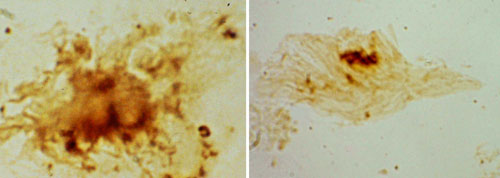
Judith: During the last 25 years we studied Borrelia burgdorferi infection in chronic or late Lyme disease. We have published pathological confirmation of the direct involvement of Borrelia burgdorferi in the two major forms of chronic/late Lyme neuroborreliosis, namely the meningovascular form associated with cerebrovascular infarcts and the atrophic form of Lyme meningoencephalitis, associated with cortical atrophy and dementia. We have also reported data on persisting typical as well as atypical and cystic forms of Borrelia burgdorferi in the brains of patients suffering from chronic Lyme neuroborreliosis. We have also shown that Borrelia spirochetes cultivated from the brains of these patients remain virulent and cause apoptosis. Furthermore, we were able to reproduce in vitro the pathological hallmarks of the atrophic form of chronic Lyme meningoencephalitis.
Whether spirochetes persist in host tissues and play a direct role in the late/chronic manifestations of syphilis was also the subject of a long debate in the history of syphilis. The detection of persisting spirochetes in brains of patients suffering from syphilitic meningoencephalitis (general paresis) ended the debate and confirmed the spirochetal origin of the late/chronic neuropsychiatric manifestations of neurosyphilis.

Today, the question as to whether Borrelia spirochetes persist is at the center of debate with respect to Lyme disease. In order to solve the debate, we reviewed the substantial amounts of data accumulated during the last 30 years with respect to chronic/late Lyme disease. The data clearly shows that the major late/chronic forms of Lyme neuroborreliosis (meningovascular and meningoencephalitis) were clinically and pathologically confirmed and Borrelia burgdorferi was detected in tertiary brain lesions and/or cultivated from the affected brain or cerebrospinal fluid. These observations were made by many authors and in various countries including the USA and Europe. Borrelia burgdorferi is able to evade destruction by the host immune reactions, persist in host tissues and sustain chronic infection and inflammation. As published in the prestigious Handbook of Clinical Neurology, these observations represent evidences that Borrelia burgdorferi in an analogous way to Treponema pallidum is responsible for the chronic/late manifestations of Lyme neuroborreliosis.
Importantly, the existence of late Lyme disease is approved by all official guidelines in the U.S., Canada and Europe. The terms "late" and "chronic" Lyme disease, as in syphilis, are synonymous and define tertiary Lyme disease. The use of "chronic" Lyme disease as a different entity is inaccurate and confusing.
Judith, to what research do you believe scientists around the world must give priority in order to better treat patients suffering from tick-borne illnesses?
Improvement of existing, and development of new efficient diagnostic tests and therapies for Lyme disease and for the various co-infections is necessary.
Detection of Borrelia burgdorferi in infected tissues and pathological confirmation of the direct role of spirochetal infection in various other chronic/late manifestations of Lyme disease is strongly warranted. Necessity of careful consideration of Borrelia burgdorferi infection in the etiology of stroke, dementia, mood disorders and the various other late/chronic manifestations of Lyme disease would be fundamental.
Despite the fact that antibiotic therapy is less efficient in chronic/late Lyme neuroborreliosis, improvement of the neuropsychiatric symptoms or complete recovery of patients was repeatedly reported, underlying the necessity of an adequate treatment. We should not forget that syphilis was almost completely eradicated by the use of Penicillin.
We have all the human experts and technological tools available to further improve and accelerate the research needed for Lyme disease, however, the most important condition, the financial support, is lacking.
Respectful open discussions, exchange and spread of knowledge between experts from all branches of medicine and sciences involved in Lyme disease research would be fundamental.
Brian, what do you believe is possible to accomplish in terms of research results by 2018?
By 2018, we will have much better diagnostic tests, including tests that will enable us to more sensitively identify current infection. We will have a new vaccine by then - one which is easier to deliver and safer as well. Finally, by 2018, we will have better treatments for patients with chronic symptoms -- and we will have biomarkers that help us to choose and target our treatments more appropriately. Patients with chronic symptoms will have many more choices than they do today.
The Global Search for Education Community Page
C. M. Rubin is the author of two widely read online series for which she received a 2011 Upton Sinclair award, "The Global Search for Education" and "How Will We Read?" She is also the author of three bestselling books, including The Real Alice in Wonderland.

No comments:
Post a Comment