Swine influenza, also called
pig influenza,
swine flu,
hog flu and
pig flu, is an infection caused by any one of several types of swine influenza
viruses.
Swine influenza virus (
SIV) or
swine-origin influenza virus (
S-OIV) is any strain of the
influenza family of viruses that is
endemic in
pigs.
[2] As of 2009, the known SIV strains include
influenza C and the subtypes of
influenza A known as
H1N1,
H1N2, H2N1,
H3N1,
H3N2, and
H2N3.
Swine influenza virus is common throughout pig populations worldwide.
Transmission of the virus from pigs to humans is not common and does
not always lead to
human flu, often resulting only in the production of
antibodies in the blood. If transmission does cause human flu, it is called
zoonotic swine flu. People with regular exposure to pigs are at increased risk of swine flu infection.
Around the mid-20th century, identification of influenza subtypes
became possible, allowing accurate diagnosis of transmission to humans.
Since then, only 50 such transmissions have been confirmed. These
strains of swine flu rarely pass from human to human. Symptoms of
zoonotic swine flu in humans are similar to those of
influenza and of
influenza-like illness in general, namely
chills,
fever,
sore throat,
muscle pains, severe
headache,
coughing,
weakness and
general discomfort.
In August 2010, the
World Health Organization declared the swine flu
pandemic officially over.
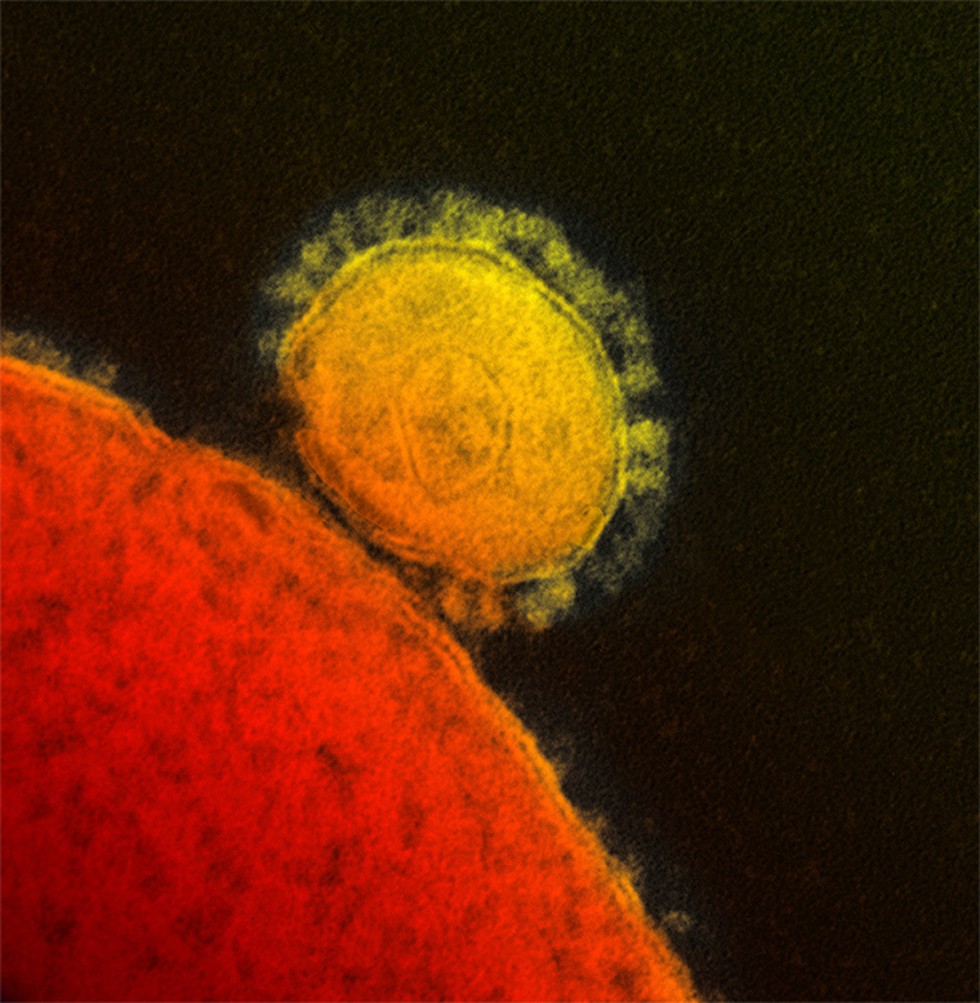
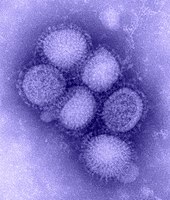
Structure
The influenza
virion
is roughly spherical. It is an enveloped virus; the outer layer is a
lipid membrane which is taken from the host cell in which the virus
multiplies. Inserted into the lipid membrane are ‘spikes’, which are
proteins – actually glycoproteins, because they consist of protein
linked to sugars – known as HA (hemagglutinin) and NA (neuraminidase).
These are the proteins that determine the subtype of influenza virus
(A/H1N1, for example). The HA and NA are important in the immune
response against the virus; antibodies (proteins made to combat
infection) against these spikes may protect against infection. The NA
protein is the target of the antiviral drugs
Relenza and
Tamiflu. Also embedded in the lipid membrane is the M2 protein, which is the target of the
antiviral adamantanes amantadine and
rimantadine.
Classification
Of the three
genera of influenza viruses that cause
human flu, two also cause influenza in pigs, with
influenza A being common in pigs and
influenza C being rare.
[3] Influenza B
has not been reported in pigs. Within influenza A and influenza C, the
strains found in pigs and humans are largely distinct, although because
of
reassortment there have been transfers of genes among strains crossing swine, avian, and human species boundaries.
Influenza C
Influenza viruses infect both humans and pigs, but do not infect birds.
[4] Transmission between pigs and humans have occurred in the past.
[5] For example, influenza C caused small outbreaks of a mild form of influenza amongst children in Japan
[6] and California.
[6]
Because of its limited host range and the lack of genetic diversity in
influenza C, this form of influenza does not cause pandemics in humans.
[7]
Influenza A
Swine influenza is known to be caused by influenza A subtypes
H1N1,
[8] H1N2,
[8] H2N3,
[9] H3N1,
[10] and
H3N2.
[8] In pigs, four influenza A virus subtypes (H1N1, H1N2,H3N2 and H7N9) are the most common strains worldwide.
[11] In the
United States,
the H1N1 subtype was exclusively prevalent among swine populations
before 1998; however, since late August 1998, H3N2 subtypes have been
isolated from pigs. As of 2004, H3N2 virus isolates in US swine and
turkey stocks were triple
reassortants, containing genes from
human (HA, NA, and PB1), swine (NS, NP, and M), and
avian (PB2 and PA) lineages.
[12]
In August 2012, the Center for Disease Control and Prevention confirmed
145 human cases (113 in Indiana, 30 in Ohio, one in Hawaii and one in
Illinois) of H3N2v since July 2012.
[13] The death of a 61-year-old
Madison County, Ohio
woman is the first in the nation associated with a new swine flu
strain. She contracted the illness after having contact with hogs at the
Ross County Fair.
[14]
Surveillance
Although there is no formal national surveillance system in the United States to determine what viruses are circulating in pigs,
[15] an informal surveillance network in the United States is part of a world surveillance network.
[16]
History
Swine influenza was first proposed to be a disease related to human flu during the
1918 flu pandemic, when pigs became ill at the same time as humans.
[17] The first identification of an influenza virus as a cause of disease in pigs occurred about ten years later, in 1930.
[18]
For the following 60 years, swine influenza strains were almost
exclusively H1N1. Then, between 1997 and 2002, new strains of three
different subtypes and five different genotypes emerged as causes of
influenza among pigs in North America. In 1997–1998,
H3N2 strains emerged. These strains, which include genes derived by
reassortment
from human, swine and avian viruses, have become a major cause of swine
influenza in North America. Reassortment between H1N1 and
H3N2 produced
H1N2. In 1999 in Canada, a strain of
H4N6 crossed the species barrier from birds to pigs, but was contained on a single farm.
[18]
The H1N1 form of swine flu is one of the descendants of the strain that caused the
1918 flu pandemic.
[19][20]
As well as persisting in pigs, the descendants of the 1918 virus have
also circulated in humans through the 20th century, contributing to the
normal seasonal epidemics of influenza.
[20] However, direct transmission from pigs to humans is rare, with only 12 recorded cases in the U.S. since 2005.
[21]
Nevertheless, the retention of influenza strains in pigs after these
strains have disappeared from the human population might make pigs a
reservoir where influenza viruses could persist, later emerging to
reinfect humans once human immunity to these strains has waned.
[22]
Swine flu has been reported numerous times as a
zoonosis
in humans, usually with limited distribution, rarely with a widespread
distribution. Outbreaks in swine are common and cause significant
economic losses in industry, primarily by causing stunting and extended
time to market. For example, this disease costs the British meat
industry about £65 million every year.
[23]
1918 pandemic in human
The
1918 flu pandemic in humans was associated with H1N1 and influenza appearing in pigs;
[20] this may reflect a
zoonosis
either from swine to humans, or from humans to swine. Although it is
not certain in which direction the virus was transferred, some evidence
suggests, in this case, pigs caught the disease from humans.
[17]
For instance, swine influenza was only noted as a new disease of pigs
in 1918, after the first large outbreaks of influenza amongst people.
[17] Although a recent
phylogenetic
analysis of more recent strains of influenza in humans, birds, and
swine suggests the 1918 outbreak in humans followed a reassortment event
within a mammal,
[24] the exact origin of the 1918 strain remains elusive.
[25] It is estimated that anywhere from 50 to 100 million people were killed worldwide.
[20][26]
1976 U.S. outbreak
On February 5, 1976, a United States army recruit at
Fort Dix
said he felt tired and weak. He died the next day, and four of his
fellow soldiers were later hospitalized. Two weeks after his death,
health officials announced the cause of death was a new strain of swine
flu. The strain, a variant of H1N1, is known as A/New Jersey/1976
(H1N1). It was detected only from January 19 to February 9 and did not
spread beyond Fort Dix.
[27]

U.S. President Ford receives a swine flu vaccination
This new strain appeared to be closely related to the strain involved
in the 1918 flu pandemic. Moreover, the ensuing increased surveillance
uncovered another strain in circulation in the U.S.:
A/Victoria/75 (H3N2) spread simultaneously, also caused illness, and persisted until March.
[27] Alarmed public health officials decided action must be taken to head off another major pandemic, and urged President
Gerald Ford that every person in the U.S. be vaccinated for the disease.
[28]
The
vaccination program was plagued by delays and public relations problems.
[29]
On October 1, 1976, immunizations began, and three senior citizens died
soon after receiving their injections. This resulted in a media outcry
that linked these deaths to the immunizations, despite the lack of any
proof the vaccine was the cause. According to science writer Patrick Di
Justo, however, by the time the truth was known—that the deaths were not
proven to be related to the vaccine—it was too late. "The government
had long feared mass panic about swine flu—now they feared mass panic
about the swine flu vaccinations." This became a strong setback to the
program.
[30]
There were reports of
Guillain-Barré syndrome, a paralyzing
neuromuscular
disorder, affecting some people who had received swine flu
immunizations. Although if a link exists is still not clear, this
syndrome may be a side effect of influenza vaccines. As a result, Di
Justo writes, "the public refused to trust a government-operated health
program that killed old people and crippled young people." In total,
48,161,019 Americans, or just over 22% of the population, had been
immunized by the time the
National Influenza Immunization Program was effectively halted on December 16, 1976.
[31] [32]
Overall, there were 1098 cases of Guillain-Barré Syndrome (GBS)
recorded nationwide by CDC surveillance, 532 of which occurred after
vaccination and 543 before vaccination.
[33] About one to two cases per 100,000 people of GBS occur every year, whether or not people have been vaccinated.
[34]
The vaccination program seems to have increased this normal risk of
developing GBS by about to one extra case per 100,000 vaccinations.
[34]
Recompensation charges were filed for over 4000 cases of severe
vaccination damage, including 25 deaths, totalling US$ 3.5 billion, by
1979.
[35] The CDC stated most studies on modern influenza vaccines have seen no link with GBS,
[34][36][37] Although one review gives an incidence of about one case per million vaccinations,
[38] a large study in China, reported in the
NEJM,
covering close to 100 million doses of H1N1 flu vaccine, found only 11
cases of Guillain-Barre syndrome, which is lower than the normal rate of
the disease in China; "The risk-benefit ratio, which is what vaccines
and everything in medicine is about, is overwhelmingly in favor of
vaccination."
[39]
1988 zoonosis
In September 1988, a swine flu virus killed one woman and infected
others. A 32-year old woman, Barbara Ann Wieners, was eight months
pregnant when she and her husband, Ed, became ill after visiting the hog
barn at a county fair in
Walworth County, Wisconsin. Barbara died eight days later, after developing pneumonia.
[40] The only pathogen identified was an H1N1 strain of swine influenza virus.
[41] Doctors were able to induce labor and deliver a healthy daughter before she died. Her husband recovered from his symptoms.
Influenza-like illness
(ILI) was reportedly widespread among the pigs exhibited at the fair.
Of the 25 swine exhibitors aged 9 to 19 at the fair, 19 tested positive
for antibodies to SIV, but no serious illnesses were seen. The virus was
able to spread between people, since one to three health care personnel
who had cared for the pregnant woman developed mild, influenza-like
illnesses, and antibody tests suggested they had been infected with
swine flu, but there was no community outbreak.
[42][43]
1998 US outbreak in swine
In 1998, swine flu was found in pigs in four U.S. states. Within a
year, it had spread through pig populations across the United States.
Scientists found this virus had originated in pigs as a recombinant form
of flu strains from birds and humans. This outbreak confirmed that pigs
can serve as a crucible where novel influenza viruses emerge as a
result of the reassortment of genes from different strains.
[44][45][46]
Genetic components of these 1998 triple-hybrid stains would later form
six out of the eight viral gene segments in the 2009 flu outbreak.
[47][48][49][50][51]
2007 Philippine outbreak in swine
![[icon]](http://upload.wikimedia.org/wikipedia/commons/thumb/1/1c/Wiki_letter_w_cropped.svg/20px-Wiki_letter_w_cropped.svg.png) |
This section requires expansion. (April 2009) |
On August 20, 2007, the Department of Agriculture officers investigated the outbreak (
epizootic) of swine flu in
Nueva Ecija and central
Luzon, Philippines. The mortality rate is less than 10% for swine flu, unless there are complications like
hog cholera. On July 27, 2007, the Philippine National Meat Inspection Service (NMIS) raised a hog cholera "red alert" warning over
Metro Manila and five regions of Luzon after the disease spread to backyard pig farms in
Bulacan and
Pampanga, even if these tested negative for the swine flu virus.
[52][53]
2009 Northern Ireland outbreak in swine
Since November 2009, 14 deaths as a result of swine flu in Northern
Ireland have been reported. The majority of the victims were reported to
have pre-existing health conditions which had lowered their immunity.
This closely corresponds to the 19 patients who had died in the year
prior due to swine flu, where 18 of the 19 were determined to have
lowered immune systems. Because of this, many mothers who have just
given birth are strongly encouraged to get a flu shot because their
immune systems are vulnerable. Also, studies have shown that people
between the ages of 15 and 44 have the highest rate of infection.
Although most people now recover, having any conditions that lower one's
immune system increases the risk of having the flu become potentially
lethal. In Northern Ireland now, approximately 56% of all people under
65 who are entitled to the vaccine have gotten the shot, and the
outbreak is said to be under control.
[54]
H1N1 virus pandemic history
A study conducted in 2009, and published in the journal
Nature, has managed to establish the evolutionary origin of the flu strain of swine origin (S-OIV).
[55]
The phylogenetic origin of the flu virus that caused the 2009
pandemics can be traced before 1918. Around 1918, the ancestral virus,
of avian origin, crossed the species boundaries and infected humans as
human H1N1. The same phenomenon took place soon after in America, where
the human virus was infecting pigs; it led to the emergence of the H1N1
swine strain, which later became the classic swine flu.
New events of reassortment were not reported until 1968, when the
avian strain H1N1 infected humans again; this time the virus met the
strain H2N2, and the reassortment originated the strain H3N2. This
strain has remained as a stable flu strain until now.
The mid-1970s were important for the evolution of flu strains. First,
the re-emergence of the human H1N1 strain became a seasonal strain.
Then, a small outbreak of swine H1N1 occurred in humans, and finally,
the human H2N2 strain apparently became extinct. Around 1979, the avian
H1N1 strain infected pigs and gave rise to Euroasiatic swine flu and
H1N1 Euroasiatic swine virus, which is still being transmitted in swine
populations.
The critical moment for the 2009 outbreak was between 1990 and 1993. A
triple reassortment event in a pig host of North American H1N1 swine
virus, the human H3N2 virus and avian H1N1 virus generated the swine
H1N2 strain. Finally, the last step in S-OIV history was in 2009, when
the virus H1N2 co-infected a human host at the same time as the
Euroasiatic H1N1 swine strain. This led to the emergence of a new human
H1N1 strain, which caused the 2009 pandemic.
On June 11, 2009, the World Health Organization raised the worldwide
pandemic alert level to Phase 6 for swine flu, which is the highest
alert level.
[56]
This alert level means that the swine flu had spread worldwide and
there were cases of people with the virus in most countries. The
pandemic level identifies the spread of the disease or virus and not
necessarily the severity of the disease.
Swine flu spread very rapidly worldwide due to its high human-to-human transmission rate and due to the frequency of air travel.
[56]
Transmission
Transmission between pigs
Influenza is quite common in pigs, with about half of breeding pigs having been exposed to the virus in the US.
[57] Antibodies to the virus are also common in pigs in other countries.
[57]
The main route of transmission is through direct contact between infected and uninfected animals.
[11] These close contacts are particularly common during animal transport.
Intensive farming may also increase the risk of transmission, as the pigs are raised in very close proximity to each other.
[58][59]
The direct transfer of the virus probably occurs either by pigs
touching noses, or through dried mucus. Airborne transmission through
the aerosols produced by pigs coughing or sneezing are also an important
means of infection.
[11] The virus usually spreads quickly through a herd, infecting all the pigs within just a few days.
[2] Transmission may also occur through wild animals, such as
wild boar, which can spread the disease between farms.
[60]
Transmission to humans
People who work with poultry and swine, especially those with intense exposures, are at increased risk of
zoonotic infection with influenza virus endemic in these animals, and constitute a population of human hosts in which
zoonosis and
reassortment can co-occur.
[61]
Vaccination of these workers against influenza and surveillance for new
influenza strains among this population may therefore be an important
public health measure.
[62]
Transmission of influenza from swine to humans who work with swine was
documented in a small surveillance study performed in 2004 at the
University of Iowa.
[63]
This study, among others, forms the basis of a recommendation that
people whose jobs involve handling poultry and swine be the focus of
increased public health surveillance.
[61]
Other professions at particular risk of infection are veterinarians and
meat processing workers, although the risk of infection for both of
these groups is lower than that of farm workers.
[64]
Interaction with avian H5N1 in pigs
Pigs are unusual as they can be infected with influenza strains that
usually infect three different species: pigs, birds and humans.
[65] This makes pigs a host where influenza viruses might exchange genes, producing new and dangerous strains.
[65] Avian influenza virus
H3N2 is
endemic in
pigs in China, and has been detected in pigs in Vietnam, increasing fears of the emergence of new variant strains.
[66] H3N2 evolved from
H2N2 by
antigenic shift.
[67] In August 2004, researchers in China found
H5N1 in pigs.
[68]
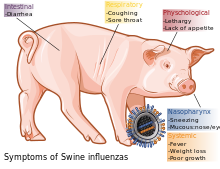
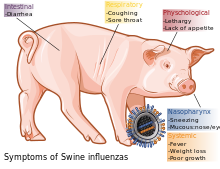
Main symptoms of swine flu in swine
[2]
These H5N1 infections may be quite common; in a survey of 10 apparently healthy pigs housed near poultry farms in
West Java,
where avian flu had broken out, five of the pig samples contained the
H5N1 virus. The Indonesian government has since found similar results in
the same region. Additional tests of 150 pigs outside the area were
negative.
[69][70]
Signs and symptoms
In swine
In pigs, influenza infection produces
fever,
lethargy,
sneezing,
coughing,
difficulty breathing and decreased appetite.
[11] In some cases the infection can cause
abortion. Although mortality is usually low (around 1–4%),
[2] the virus can produce
weight loss and
poor growth, causing economic loss to farmers.
[11] Infected pigs can lose up to 12 pounds of body weight over a three- to four-week period.
[11]
In humans

Main symptoms of swine flu in humans
[71]
Direct transmission of a swine flu virus from pigs to humans is occasionally possible (called
zoonotic
swine flu). In all, 50 cases are known to have occurred since the first
report in medical literature in 1958, which have resulted in a total of
six deaths.
[72] Of these six people, one was pregnant, one had
leukemia, one had
Hodgkin's lymphoma and two were known to be previously healthy.
[72]
Despite these apparently low numbers of infections, the true rate of
infection may be higher, since most cases only cause a very mild
disease, and will probably never be reported or diagnosed.
[72]
In this video, Dr. Joe Bresee, with CDC's Influenza Division, describes
the symptoms of swine flu and warning signs to look for that indicate
the need for urgent medical attention.
See also: See this video with subtitles on YouTube
[73]
According to the
Centers for Disease Control and Prevention (CDC), in humans the symptoms of the 2009 "swine flu" H1N1 virus are similar to those of
influenza and of
influenza-like illness in general. Symptoms include
fever,
cough,
sore throat, body aches,
headache,
chills and
fatigue. The 2009 outbreak has shown an increased percentage of patients reporting
diarrhea and
vomiting.
[74] The 2009 H1N1 virus is not zoonotic swine flu, as it is not transmitted from pigs to humans, but from person to person.
Because these symptoms are not specific to swine flu, a
differential diagnosis of
probable
swine flu requires not only symptoms, but also a high likelihood of
swine flu due to the person's recent history. For example, during the
2009 swine flu outbreak in the United States, the CDC advised physicians to "consider swine influenza infection in the differential diagnosis of patients with
acute febrile respiratory illness
who have either been in contact with persons with confirmed swine flu,
or who were in one of the five U.S. states that have reported swine flu
cases or in Mexico during the seven days preceding their illness onset."
[75] A diagnosis of
confirmed swine flu requires laboratory testing of a respiratory sample (a simple nose and throat swab).
[75]
The most common cause of death is
respiratory failure. Other causes of death are
pneumonia (leading to
sepsis),
[76] high fever (leading to neurological problems),
dehydration (from excessive vomiting and
diarrhea),
electrolyte imbalance and
kidney failure.
[77] Fatalities are more likely in young children and the elderly.
Diagnosis
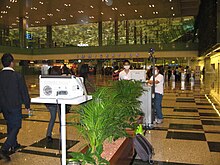
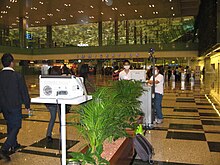
Thermal scanning of passengers arriving at Singapore Changi airport
The CDC recommends
real time PCR as the method of choice for diagnosing H1N1.
[78] This method allows a specific diagnosis of novel influenza (H1N1) as opposed to
seasonal influenza. Near-patient
point-of-care tests are in development.
[79]
Prevention
Prevention of swine influenza has three components: prevention in
swine, prevention of transmission to humans, and prevention of its
spread among humans.
In swine
Methods of preventing the spread of influenza among swine include facility management, herd management, and vaccination (
ATCvet code:
QI09AA03).
Because much of the illness and death associated with swine flu
involves secondary infection by other pathogens, control strategies that
rely on vaccination may be insufficient.
Control of swine influenza by vaccination has become more difficult in recent decades, as the
evolution of the
virus
has resulted in inconsistent responses to traditional vaccines.
Standard commercial swine flu vaccines are effective in controlling the
infection when the virus strains match enough to have significant
cross-protection, and custom (autogenous) vaccines made from the
specific viruses isolated are created and used in the more difficult
cases.
[80][81] Present
vaccination
strategies for SIV control and prevention in swine farms typically
include the use of one of several bivalent SIV vaccines commercially
available in the United States. Of the 97 recent H3N2 isolates examined,
only 41 isolates had strong serologic cross-reactions with antiserum to
three commercial SIV vaccines. Since the protective ability of
influenza vaccines depends primarily on the closeness of the match
between the vaccine virus and the epidemic virus, the presence of
nonreactive H3N2 SIV variants suggests current commercial vaccines might
not effectively protect pigs from infection with a majority of H3N2
viruses.
[72][82]
The United States Department of Agriculture researchers say while pig
vaccination keeps pigs from getting sick, it does not block infection or
shedding of the virus.
[83]
Facility management includes using disinfectants and ambient
temperature to control viruses in the environment. They are unlikely to
survive outside living cells for more than two weeks, except in cold
(but above freezing) conditions, and are readily inactivated by
disinfectants.
[2]
Herd management includes not adding pigs carrying influenza to herds
that have not been exposed to the virus. The virus survives in healthy
carrier pigs for up to three months, and can be recovered from them
between outbreaks. Carrier pigs are usually responsible for the
introduction of SIV into previously uninfected herds and countries, so
new animals should be
quarantined.
[57] After an outbreak, as immunity in exposed pigs wanes, new outbreaks of the same strain can occur.
[2]
In humans
- Prevention of pig-to-human transmission
Swine can be infected by both avian and human flu strains of influenza, and therefore are hosts where the
antigenic shifts can occur that create new influenza strains.
The transmission from swine to humans is believed to occur mainly in
swine farms, where farmers are in close contact with live pigs. Although
strains of swine influenza are usually not able to infect humans, this
may occasionally happen, so farmers and veterinarians are encouraged to
use face
masks
when dealing with infected animals. The use of vaccines on swine to
prevent their infection is a major method of limiting swine-to-human
transmission. Risk factors that may contribute to swine-to-human
transmission include smoking and, especially, not wearing gloves when
working with sick animals, thereby increasing the likelihood of
subsequent hand-to-eye, hand-to-nose or hand-to-mouth transmission.
[84]
- Prevention of human-to-human transmission
Influenza spreads between humans when infected people cough or
sneeze, then other people breathe in the virus or touch something with
the virus on it and then touch their own face.
[85] "Avoid touching your eyes, nose or mouth. Germs spread this way."
[86] Swine flu cannot be spread by pork products, since the virus is not transmitted through food.
[85]
The swine flu in humans is most contagious during the first five days
of the illness, although some people, most commonly children, can remain
contagious for up to ten days. Diagnosis can be made by sending a
specimen, collected during the first five days, for analysis.
[87]

Thermal imaging camera and screen, photographed in an airport terminal
in Greece - thermal imaging can detect elevated body temperature, one of
the signs of the virus H1N1 (swine influenza).
Recommendations to prevent spread of the virus among humans include using standard
infection control, which includes frequent washing of hands with soap and water or with
alcohol-based hand sanitizers, especially after being out in public.
[88]
Chance of transmission is also reduced by disinfecting household
surfaces, which can be done effectively with a diluted chlorine bleach
solution.
[89]
Experts agree hand-washing can help prevent viral infections,
including ordinary and the swine flu infections. Also, avoiding touching
one's eyes, nose or mouth with one's hands helps to prevent the flu.
[86]
Influenza can spread in coughs or sneezes, but an increasing body of
evidence shows small droplets containing the virus can linger on
tabletops, telephones and other surfaces and be transferred via the
fingers to the eyes, nose or mouth.
Alcohol-based gel or foam hand sanitizers
work well to destroy viruses and bacteria. Anyone with flu-like
symptoms, such as a sudden fever, cough or muscle aches, should stay
away from work or public transportation, and should contact a doctor for
advice.
[90]
Social distancing,
another tactic, is staying away from other people who might be
infected, and can include avoiding large gatherings, spreading out a
little at work, or perhaps staying home and lying low if an infection is
spreading in a community.
Public health
and other responsible authorities have action plans which may request
or require social distancing actions, depending on the severity of the
outbreak.
Vaccination
Vaccines are available for different kinds of swine flu. The U.S.
Food and Drug Administration (FDA) approved the new swine flu vaccine for use in the United States on September 15, 2009.
[91] Studies by the
National Institutes of Health show a single dose creates enough antibodies to protect against the virus within about 10 days.
[92]
In the aftermath of the 2009 pandemic, several studies were conducted
to see who received influenza vaccines. These studies show that whites
are much more likely to be vaccinated for seasonal influenza and for the
H1N1 strain than African Americans
[93]
This could be due to several factors. Historically, there has been
mistrust of vaccines and of the medical community from African
Americans. Many African Americans do not believe vaccines or doctors to
be effective. This mistrust stems from the exploitation of the African
American communities during studies like the Tuskegee study.
Additionally, vaccines are typically administered in clinics, hospitals,
or doctor’s offices. Many people of lower socioeconomic status are less
likely to receive vaccinations because they do not have health
insurance.
Treatment
In swine
As swine influenza is rarely fatal to pigs, little treatment beyond rest and supportive care is required.
[57] Instead, veterinary efforts are focused on preventing the spread of the virus throughout the farm, or to other farms.
[11]
Vaccination and animal management techniques are most important in
these efforts. Antibiotics are also used to treat this disease, which
although they have no effect against the influenza virus, do help
prevent bacterial
pneumonia and other
secondary infections in influenza-weakened herds.
[57]
In humans
If a person becomes sick with swine flu, antiviral drugs can make the
illness milder and make the patient feel better faster. They may also
prevent serious flu complications. For treatment, antiviral drugs work
best if started soon after getting sick (within two days of symptoms).
Beside antivirals, supportive care at home or in a hospital focuses on
controlling fevers, relieving pain and maintaining fluid balance, as
well as identifying and treating any secondary infections or other
medical problems. The U.S.
Centers for Disease Control and Prevention recommends the use of
oseltamivir (Tamiflu) or
zanamivir
(Relenza) for the treatment and/or prevention of infection with swine
influenza viruses; however, the majority of people infected with the
virus make a full recovery without requiring medical attention or
antiviral drugs.
[94] The virus isolated in the 2009 outbreak have been found resistant to
amantadine and
rimantadine.
[95]
In the U.S., on April 27, 2009, the FDA issued
Emergency Use Authorizations to make available
Relenza and
Tamiflu antiviral drugs
to treat the swine influenza virus in cases for which they are
currently unapproved. The agency issued these EUAs to allow treatment of
patients younger than the current approval allows and to allow the
widespread distribution of the drugs, including by volunteers.
[96]
See also