From Wikipedia, the free encyclopedia
 |
|
|---|---|
| Vaccine description | |
| Target disease | Polio virus |
| Type | ? |
| Clinical data | |
| AHFS/Drugs.com | Multum Consumer Information |
| Pregnancy cat. | C (both OPV and IPV) |
| Legal status | Administered by or under the supervision of a health care professional. |
| Routes | Parenteral (IPV), Oral drops (OPV) |
| Identifiers | |
| ATC code | J07BF01 J07BF02 J07BF03 |
| |
|
Contents
Development
In generic sense, vaccination works by priming the immune system with an 'immunogen'. Stimulating immune response, via use of an infectious agent, is known as immunization. The development of immunity to polio efficiently blocks person-to-person transmission of wild poliovirus, thereby protecting both individual vaccine recipients and the wider community.[3]In 1936, Maurice Brodie, a research assistant at New York University, attempted to produce a formaldehyde-killed polio vaccine from ground-up monkey spinal cords. His initial attempts were hampered by the difficulty of obtaining enough virus. Brodie first tested the vaccine on himself and several of his assistants. He then gave the vaccine to three thousand children. Many of these children developed allergic reactions, but none developed immunity to polio.[8] Philadelphia pathologist John Kolmer also claimed to have developed a vaccine that same year, but it too produced no immunity and was blamed for causing cases of paralytic polio, nine of them fatal.[9]

Mass polio vaccination in Columbus, Georgia during the early days of the National Polio Immunization Program.
This development greatly facilitated vaccine research and ultimately allowed for the development of vaccines against polio. Enders and his colleagues, Thomas H. Weller and Frederick C. Robbins, were recognized in 1954 for their labors with a Nobel Prize in Physiology or Medicine.[11] Other important advances that led to the development of polio vaccines were: the identification of three poliovirus serotypes (Poliovirus type 1 — PV1, or Mahoney; PV2, Lansing; and PV3, Leon); the finding that prior to paralysis, the virus must be present in the blood; and the demonstration that administration of antibodies in the form of gamma-globulin protects against paralytic polio.[12][13]
In 1952 and 1953, the U.S. experienced an outbreak of 58,000 and 35,000 polio cases, respectively, up from a typical number of some 20,000 a year. Amid this U.S. polio epidemic, millions of dollars were invested in finding and marketing a polio vaccine by commercial interests, including Lederle Laboratories in New York under the direction of H. R. Cox. Also working at Lederle was Polish-born virologist and immunologist Hilary Koprowski, who claims to have created the first successful polio vaccine, in 1950. His vaccine, however, being a live attenuated virus taken orally, was still in the research stage and would not be ready for use until five years after Jonas Salk's polio vaccine (a dead-virus injectable vaccine) had reached the market. Koprowski's attenuated vaccine was prepared by successive passages through the brains of Swiss albino mice. By the seventh passage, the vaccine strains could no longer infect nervous tissue or cause paralysis. After one to three further passages on rats, the vaccine was deemed safe for human use.[14][15] On February 27, 1950, Koprowski's live, attenuated vaccine was tested for the first time on an 8-year-old boy living at Letchworth Village, an institution for the physically and mentally disabled located in New York. After the child suffered no side effects, Koprowski enlarged his experiment to include 19 other children.[14][16]
The development of two polio vaccines led to the first modern mass inoculations. The last cases of paralytic poliomyelitis caused by endemic transmission of wild virus in the United States occurred in 1979, with an outbreak among the Amish in several Midwest states.[17] A global effort to eradicate polio, led by the World Health Organization, UNICEF, and The Rotary Foundation, began in 1988 and has relied largely on the oral polio vaccine developed by Albert Sabin.[18] The disease was entirely eradicated in the Americas by 1994.[19] Polio was officially eradicated in 36 Western Pacific countries, including China and Australia in 2000.[20][21] Europe was declared polio-free in 2002.[22] Since January 2011, there were no reported cases of the disease in India, and hence in February 2012, the country was taken off the WHO list of polio endemic countries. It is reported that if there are no cases of polio in the country for two more years, it will be declared as a polio-free country.[23][24] As of 2008, polio remains endemic in only three countries: Nigeria, Pakistan, and Afghanistan.[25][26] Although poliovirus transmission has been interrupted in much of the world, transmission of wild poliovirus does continue and creates an ongoing risk for the importation of wild poliovirus into previously polio-free regions. If importations of poliovirus occurs, outbreaks of poliomyelitis may develop, especially in areas with low vaccination coverage and poor sanitation. As a result, high levels of vaccination coverage must be maintained.[19]
Inactivated vaccine

Administration of the polio inoculation, including by Salk himself, in 1957 at the University of Pittsburgh where he and his team had developed the vaccine
The Salk vaccine, or inactivated poliovirus vaccine (IPV), is based on three wild, virulent reference strains, Mahoney (type 1 poliovirus), MEF-1 (type 2 poliovirus), and Saukett (type 3 poliovirus), grown in a type of monkey kidney tissue culture (Vero cell line), which are then inactivated with formalin.[12] The injected Salk vaccine confers IgG-mediated immunity in the bloodstream, which prevents polio infection from progressing to viremia and protects the motor neurons, thus eliminating the risk of bulbar polio and post-polio syndrome.
Beginning February 23, 1954, the vaccine was tested at Arsenal Elementary School and the Watson Home for Children in Pittsburgh, Pennsylvania.[28] Salk's vaccine was then used in a test called the Francis Field Trial, led by Thomas Francis; the largest medical experiment in history. The test began with some 4,000 children at Franklin Sherman Elementary School in McLean, Virginia,[29] and would eventually involve 1.8 million children, in 44 states from Maine to California.[30] By the conclusion of the study, roughly 440,000 received one or more injections of the vaccine, about 210,000 children received a placebo, consisting of harmless culture media, and 1.2 million children received no vaccination and served as a control group, who would then be observed to see if any contracted polio.[14] The results of the field trial were announced April 12, 1955 (the tenth anniversary of the death of President Franklin D. Roosevelt, whose paralysis was generally believed to have been caused by polio). The Salk vaccine had been 60–70% effective against PV1 (poliovirus type 1), over 90% effective against PV2 and PV3, and 94% effective against the development of bulbar polio.[31] Soon after Salk's vaccine was licensed in 1955 children's vaccination campaigns were launched. In the U.S, following a mass immunization campaign promoted by the March of Dimes, the annual number of polio cases fell from 35,000 in 1953 to 5,600 by 1957.[32] By 1961 only 161 cases were recorded in the United States.[33]
An enhanced-potency IPV was licensed in the United States in November 1987, and is currently the vaccine of choice in the United States.[17] The first dose of polio vaccine is given shortly after birth, usually between 1–2 months of age, a second dose is given at 4 months of age.[17] The timing of the third dose depends on the vaccine formulation but should be given between 6–18 months of age.[34] A booster vaccination is given at 4 to 6 years of age, for a total of four doses at or before school entry.[35] In some countries, a fifth vaccination is given during adolescence.[34] Routine vaccination of adults (18 years of age and older) in developed countries is neither necessary nor recommended because most adults are already immune and have a very small risk of exposure to wild poliovirus in their home countries.[17]
In 2002, a pentavalent (5-component) combination vaccine (called Pediarix) containing IPV was approved for use in the United States. The vaccine also contains combined diphtheria, tetanus, and acellular pertussis vaccines (DTaP) and a pediatric dose of hepatitis B vaccine.[17] In the UK, IPV is combined with tetanus, diphtheria, pertussis and Haemophilus influenzae type b vaccines.[34] When the current formulation of IPV is used, 90% or more of individuals develop protective antibody to all three serotypes of poliovirus after two doses of inactivated polio vaccine (IPV), and at least 99% are immune to poliovirus following three doses. The duration of immunity induced by IPV is not known with certainty, although a complete series is thought to provide protection for many years.[36]
Oral vaccine
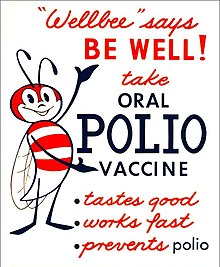
This 1963 poster featured CDC’s national symbol of public health, the "Wellbee", encouraging the public to receive an oral polio vaccine.
There are 57 nucleotide substitutions which distinguish the attenuated Sabin 1 strain from its virulent parent (the Mahoney serotype), two nucleotide substitutions attenuate the Sabin 2 strain, and 10 substitutions are involved in attenuating the Sabin 3 strain.[12] The primary attenuating factor common to all three Sabin vaccines is a mutation located in the virus's internal ribosome entry site (IRES)[40] which alters stem-loop structures, and reduces the ability of poliovirus to translate its RNA template within the host cell.[41] The attenuated poliovirus in the Sabin vaccine replicates very efficiently in the gut, the primary site of infection and replication, but is unable to replicate efficiently within nervous system tissue. OPV also proved to be superior in administration, eliminating the need for sterile syringes and making the vaccine more suitable for mass vaccination campaigns. OPV also provided longer lasting immunity than the Salk vaccine.
In 1961, type 1 and 2 monovalent oral poliovirus vaccine (MOPV) was licensed, and in 1962, type 3 MOPV was licensed. In 1963, trivalent OPV (TOPV) was licensed, and became the vaccine of choice in the United States and most other countries of the world, largely replacing the inactivated polio vaccine.[8] A second wave of mass immunizations led to a further dramatic decline in the number of polio cases. Between 1962 and 1965 about 100 million Americans (roughly 56% of the population at that time) received the Sabin vaccine. The result was a substantial reduction in the number of poliomyelitis cases, even from the much reduced levels following the introduction of the Salk vaccine.[42]
OPV is usually provided in vials containing 10-20 doses of vaccine. A single dose of oral polio vaccine (usually two drops) contains 1,000,000 infectious units of Sabin 1 (effective against PV1), 100,000 infectious units of the Sabin 2 strain, and 600,000 infectious units of Sabin 3. The vaccine contains small traces of antibiotics— neomycin and streptomycin—but does not contain preservatives.[43] One dose of OPV produces immunity to all three poliovirus serotypes in approximately 50% of recipients.[17] Three doses of live-attenuated OPV produce protective antibody to all three poliovirus types in more than 95% of recipients. OPV produces excellent immunity in the intestine, the primary site of wild poliovirus entry, which helps prevent infection with wild virus in areas where the virus is endemic.[35] The live virus used in the vaccine is shed in the stool and can be spread to others within a community. IPV produces less gastrointestinal immunity than does OPV, and primarily acts by preventing the virus from entering the nervous system. In regions without wild poliovirus, inactivated polio vaccine is the vaccine of choice.[35] In regions with higher incidence of polio, and thus a different relative risk between efficacy and reversion of the vaccine to a virulent form, live vaccine is still used. The live virus also has stringent requirements for transport and storage, which are a problem in some hot or remote areas. As with other live-virus vaccines, immunity initiated by OPV is probably lifelong.[36]
Iatrogenic (vaccine-induced) polio
A major concern about the oral polio vaccine (OPV) is its known ability to revert to a form that can achieve neurological infection and cause paralysis.[44] Clinical disease, including paralysis, caused by vaccine-derived poliovirus (VDPV) is indistinguishable from that caused by wild polioviruses.[45] This is believed to be a rare event, but outbreaks of vaccine-associated paralytic poliomyelitis (VAPP) have been reported, and tend to occur in areas of low coverage by OPV, presumably because the OPV is itself protective against the related outbreak strain.[46][47]
Doses of oral polio vaccine are added to sugar cubes for use in a 1967 vaccination campaign in Bonn, Germany
The rate of vaccine-associated paralytic poliomyelitis (VAPP) varies by region but is generally about 1 case per 750,000 vaccine recipients.[49] VAPP is more likely to occur in adults than in children. In immunodeficient children, the risk of VAPP is almost 7,000 times higher, particularly for persons with B-lymphocyte disorders (e.g., agammaglobulinemia and hypogammaglobulinemia), which reduce the synthesis of protective antibodies.[45] The World Health Organization considers the benefits of vaccination to far outweigh the risk of vaccine derived polio. Outbreaks of vaccine derived polio have been stopped by multiple rounds of high-quality vaccination, in order to immunize the entire population.[50]
Outbreaks of VAPP occurred independently in Belarus (1965–66), Canada (1966–68), Egypt (1983–1993), Hispaniola (2000–2001), Philippines (2001), Madagascar (2001–2002),[51] and in Haiti (2002), where political strife and poverty have interfered with vaccination efforts.[52] In 2006 an outbreak of vaccine-derived poliovirus occurred in China.[53] Cases have been reported from Cambodia (2005–2006), Myanmar (2006–2007), Iran (1995, 2005–2007), Syria, Kuwait and Egypt.[54] Since 2005, The World Health Organization has been tracking vaccine-caused polio in northern Nigeria caused by a mutation in live oral polio vaccines.[55]
Contamination concerns
In 1960, it was determined that the rhesus monkey kidney cells used to prepare the poliovirus vaccines were infected with the SV40 virus (Simian Virus-40).[56] SV40 was also discovered in 1960 and is a naturally occurring virus that infects monkeys. In 1961, SV40 was found to cause tumors in rodents.[57] More recently, the virus was found in certain forms of cancer in humans, for instance brain and bone tumors, pleural and peritoneal mesothelioma, and some types of non-Hodgkin's lymphoma.[58][59] However, it has not been determined that SV40 causes these cancers.[60]SV40 was found to be present in stocks of the injected form of the polio vaccine (IPV) in use between 1955 to 1963.[56] It is not found in the OPV form.[56] Over 98 million Americans received one or more doses of polio vaccine between 1955 to 1963 when a proportion of vaccine was contaminated with SV40; it has been estimated that 10–30 million Americans may have received a dose of vaccine contaminated with SV40.[56] Later analysis suggested that vaccines produced by the former Soviet bloc countries until 1980, and used in the USSR, China, Japan, and several African countries, may have been contaminated; meaning hundreds of millions more may have been exposed to SV40.[61]
In 1998, the National Cancer Institute undertook a large study, using cancer case information from the Institutes SEER database. The published findings from the study revealed that there was no increased incidence of cancer in persons who may have received vaccine containing SV40.[62] Another large study in Sweden examined cancer rates of 700,000 individuals who had received potentially contaminated polio vaccine as late as 1957; the study again revealed no increased cancer incidence between persons who received polio vaccines containing SV40 and those who did not.[63] The question of whether SV40 causes cancer in humans remains controversial however, and the development of improved assays for detection of SV40 in human tissues will be needed to resolve the controversy.[60]
During the race to develop an oral polio vaccine several large scale human trials were undertaken. By 1958, the National Institutes of Health had determined that OPV produced using the Sabin strains were the safest.[14] Between 1957 and 1960, however, Hilary Koprowski continued to administer his vaccine around the world. In Africa, the vaccines were administered to roughly one million people in the Belgian territories, now the Democratic Republic of the Congo, Rwanda and Burundi.[64][65] The results of these human trials have been controversial,[66] and accusations in the 1990s arose that the vaccine had created the conditions necessary for transmission of SIV from chimpanzees to humans, causing HIV/AIDS. These hypotheses have, however, been refuted in some studies.[64] By 2004, cases of poliomyelitis in Africa had been reduced to just a small number of isolated regions in the western portion of the continent, with sporadic cases elsewhere. However, recent opposition to vaccination campaigns has evolved,[67][68] often relating to fears that the vaccine might induce sterility.[69] The disease has since resurged in Nigeria and in several other African nations, which epidemiologists believe is due to refusals by certain local populations to allow their children to receive the polio vaccine.[70



No comments:
Post a Comment