From Wikipedia, the free encyclopedia

Disability-adjusted life year for HIV and AIDS per 100,000 inhabitants
no data
≤ 10
10–25
25–50
50–100
100–500
500–1000
1000–2500
2500–5000
5000–7500
7500-10000
10000-50000
≥ 50000
Sub-Saharan Africa is the region most affected. In 2010, an estimated 68% (22.9 million) of all HIV cases and 66% of all deaths (1.2 million) occurred in this region.[3] This means that about 5% of the adult populations is infected.[4] Here in contrast to other regions women compose nearly 60% of cases.[3] South Africa has the largest population of people with HIV of any country in the world at 5.9 million.[3]
South & South East Asia (a region with about 2 billion people as of 2010, over 30% of the global population) has an estimated 4 million cases (12% of all people living with HIV), with about 250,000 deaths in 2010.[4] Approximately 2.5 million of these cases are in India, where however the prevalence is only about 0.3% (somewhat higher than that found in Western and Central Europe or Canada).[3] Prevalence is lowest in East Asia at 0.1%.[4]
In 2008 approximately 1.2 million people in the United States had HIV; 20% did not realize that they were infected.[5] It resulted in about 17,500 deaths.[5] In the United Kingdom, as of 2009, there were approximately 86,500 cases and 516 deaths.[6] In Australia, as of 2009, there were about 21,171 cases and around 23 deaths.[7] In Canada as of 2008 there were about 65,000 cases and 53 deaths.[8]
Since AIDS was first recognized in 1981 and 2009 it has led to nearly 30 million deaths.[9]
By region
The pandemic is not homogeneous within regions, with some countries more afflicted than others. Even at the country level, there are wide variations in infection levels between different areas. The number of people infected with HIV continues to rise in most parts of the world, despite the implementation of prevention strategies, Sub-Saharan Africa being by far the worst-affected region, with an estimated 22.9 million at the end of 2010, 68% of the global total.[10]South and South East Asia have an estimated 12% of the global total.[11] The rate of new infections has fallen slightly since 2005 after a more rapid decline between 1997 and 2005.[10] Annual AIDS deaths have been continually declining since 2005 as antiretroviral therapy has become more widely available.
| World region | Estimated prevalence of HIV infection (adults and children) |
Estimated adult and child deaths during 2010 |
Adult prevalence (%) |
|---|---|---|---|
| Worldwide | 31.6 million – 35.2 million | 1.6 to 1.9 million | 0.8% |
| Sub-Saharan Africa | 21.6 million – 24.1 million | 1.2 million | 5.0% |
| South and South-East Asia | 3.6 million – 4.5 million | 250,000 | 0.3% |
| Eastern Europe and Central Asia | 1.3 million – 1.7 million | 90,000 | 0.9% |
| Latin America | 1.2 million – 1.7 million | 67,000 | 0.4% |
| North America | 1.0 million – 1.9 million | 20,000 | 0.6% |
| East Asia | 580,000 – 1.1 million | 56,000 | 0.1% |
| Western and Central Europe | 770,000 – 930,000 | 9,900 | 0.2% |
Sub-Saharan Africa
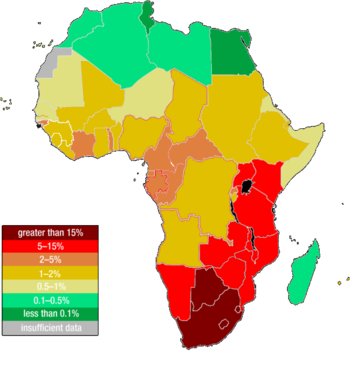
Estimated HIV infection in Africa in 2007.

Graphs of life expectancy at birth for some sub-Saharan countries
showing the fall in the 1990s primarily due to the AIDS pandemic.[12]
Main article: HIV/AIDS in Africa
Sub-Saharan Africa remains the hardest-hit region. HIV infection is becoming endemic in sub-Saharan Africa, which is home to just over 12% of the world’s population but two-thirds of all people infected with HIV.[10] The adult HIV prevalence rate is 5.0% and between 21.6 million and 24.1 million total are affected.[10] However, the actual prevalence varies between regions. Presently, Southern Africa is the hardest hit region, with adult prevalence rates exceeding 20% in most countries in the region, and 30% in Swaziland and Botswana.Eastern Africa also experiences relatively high levels of prevalence with estimates above 10% in some countries, although there are signs that the pandemic is declining in this region. West Africa on the other hand has been much less affected by the pandemic. Several countries reportedly have prevalence rates around 2 to 3%, and no country has rates above 10%. In Nigeria and Côte d'Ivoire, two of the region's most populous countries, between 5 and 7% of adults are reported to carry the virus.
Across Sub-Saharan Africa, more women are infected with HIV than men, with 13 women infected for every 10 infected men. This gender gap continues to grow. Throughout the region, women are being infected with HIV at earlier ages than men. The differences in infection levels between women and men are most pronounced among young people (aged 15–24 years). In this age group, there are 36 women infected with HIV for every 10 men. The widespread prevalence of sexually transmitted diseases, the practice of scarification, unsafe blood transfusions, and the poor state of hygiene and nutrition in some areas may all be facilitating factors in the transmission of HIV-1 (Bentwich et al., 1995).
Mother-to-child transmission is another contributing factor in the transmission of HIV-1 in developing nations. Due to a lack of testing, a shortage in antenatal therapies and through the feeding of contaminated breast milk, 590,000 infants born in developing countries are infected with HIV-1 per year. In 2000, the World Health Organization estimated that 25% of the units of blood transfused in Africa were not tested for HIV, and that 10% of HIV infections in Africa were transmitted via blood.
Poor economic conditions (leading to the use of dirty needles in healthcare clinics) and lack of sex education contribute to high rates of infection. In some African countries, 25% or more of the working adult population is HIV-positive. Poor economic conditions caused by slow onset-emergencies, such as drought, or rapid onset natural disasters and conflict can result in young women and girls being forced into using sex as a survival strategy.[13] Worse still, research indicates that as emergencies, such as drought, take their toll and the number of potential 'clients' decreases, women are forced by clients to accept greater risks, such as not using contraceptives.[13]
AIDS-denialist policies have impeded the creation of effective programs for distribution of antiretroviral drugs. Denialist policies by former South African President Thabo Mbeki's administration led to several hundred thousand unnecessary deaths.[14][15] UNAIDS estimates that in 2005 there were 5.5 million people in South Africa infected with HIV — 12.4% of the population. This was an increase of 200,000 people since 2003.
Although HIV infection rates are much lower in Nigeria than in other African countries, the size of Nigeria's population meant that by the end of 2003, there were an estimated 3.6 million people infected. On the other hand, Uganda, Zambia, Senegal, and most recently Botswana have begun intervention and educational measures to slow the spread of HIV, and Uganda has succeeded in actually reducing its HIV infection rate.
Middle East and North Africa
| This section does not cite any references or sources. (June 2008) |
South and South-East Asia
Main article: HIV/AIDS in Asia
The HIV prevalence rate in South and South-East Asia is less than
0.35 percent, with total of 4.2 – 4.7 million adults and children
infected. More AIDS deaths (480,000) occur in this region than in any
other except sub-Saharan Africa. The geographical size and human
diversity of South and South-East Asia have resulted in HIV epidemics
differing across the region. The AIDS picture in South Asia is dominated
by the epidemic in India.In South and Southeast Asia, the HIV epidemic remains largely concentrated in injecting drug users, men who have sex with men, sex workers, and clients of sex workers and their immediate sexual partners.[16] In the Philippines, in particular, sexual contact between males comprise majority of new infections. An HIV surveillance study conducted by Dr. Louie Mar Gangcuangco and colleagues from the University of the Philippines-Philippine General Hospital showed that out of 406 MSM tested for HIV in Metro Manila, HIV prevalence was 11.8% (95% confidence interval: 8.7- 15.0).[17] [18]
Migrants, in particular, are vulnerable and 67% of those infected in Bangladesh and 41% in Nepal are migrants returning from India.[16] This is in part due to human trafficking and exploitation, but also because even those migrants who willingly go to India in search of work are often afraid to access state health services due to concerns over their immigration status.[16]
East Asia
| This section does not cite any references or sources. (January 2011) |
Main article: HIV/AIDS in Asia
The national HIV prevalence levels in East Asia is 0.1% in the adult
(15–49) group. However, due to the large populations of many East Asian
nations, this low national HIV prevalence still means that large numbers
of people are infected with HIV. The picture in this region is
dominated by China. Much of the current spread of HIV in China is
through injecting drug use and paid sex. In China, the number was
estimated at between 430,000 and 1.5 million by independent researchers,
with some estimates going much higher.In the rural areas of China, where large numbers of farmers, especially in Henan province, participated in unclean blood transfusions; estimates of those infected are in the tens of thousands. In Japan, just over half of HIV/AIDS cases are officially recorded as occurring amongst homosexual men, with the remainder occurring amongst heterosexuals and also via drug abuse, in the womb or unknown means.
Americas
Caribbean
Main article: HIV/AIDS in the Caribbean
The Caribbean is the second-most affected region in the world.[10] Among adults aged 15–44, AIDS has become the leading cause of death. The region's adult prevalence rate is 0.9%.[10] with national rates ranging up to 2.7%.[19] HIV transmission occurs largely through heterosexual intercourse,[citation needed]
with two-thirds of AIDS cases in this region attributed to this route.
Sex between men is also a significant route of transmission, even though
it is heavily stigmatised and illegal in many areas. HIV transmission
through injecting drug use remains rare, except in Bermuda and Puerto
Rico.Central and South America
| This section does not cite any references or sources. (January 2011) |
Main article: HIV/AIDS in Latin America
In these regions of the American continent, only Guatemala and Honduras have national HIV prevalence of over 1%. In these countries, HIV-infected men outnumber HIV-infected women by roughly 3:1.United States and Canada
Main articles: HIV/AIDS in the United States and HIV/AIDS in Canada
The adult prevalence rate in this region is 0.7% with over 1 million
people currently infected with HIV. In the United States from 2001–2005,
the highest transmission risk behaviors were sex between men (40–49% of
new cases) and high risk heterosexual sex (32–35% of new cases).[20] Currently, rates of HIV infection in the US are highest in the eastern and southern regions, with the exception of California.
Currently, 35,000–40,000 new infections occur in the USA every year.
AIDS is one of the top three causes of death for African American men
aged 25–54 and for African American women aged 35–44 years in the United
States of America. In the United States, African Americans make up
about 48% of the total HIV-positive population and make up more than
half of new HIV cases, despite making up only 12% of the population. The
main route of transmission for women is through unprotected
heterosexual sex. African American women are 19 times more likely to
contract HIV than other women.[21] Experts[who?]
attribute this to "AIDS fatigue" among younger people who have no
memory of the worst phase of the epidemic in the 1980s and early 1990s,
as well as "condom fatigue" among those who have grown tired of and disillusioned with the unrelenting safer sex message. This trend is of major concern to public health workers.In the United States in particular, a new wave of infection is being blamed on the use of methamphetamine, known as crystal meth. Research presented at the 12th Annual Retrovirus Conference in Boston in February 2005 concluded that using crystal meth or cocaine is the biggest single risk factor for becoming HIV+ among US gay men, contributing 29% of the overall risk of becoming positive and 28% of the overall risk of being the receptive partner in anal sex.[22]
In addition, several renowned clinical psychologists now cite methamphetamine as the biggest problem facing gay men today, including Michael Majeski, who believes meth is the catalyst for at least 80% of seroconversions currently occurring across the United States, and Tony Zimbardi, who calls methamphetamine the number one cause of HIV transmission, and says that high rates of new HIV infection are not being found among non-crystal users. In addition, various HIV and STD clinics across the United States report anecdotal evidence that 75% of new HIV seroconversions they deal with are methamphetamine-related; indeed, in Los Angeles, methamphetamine is regarded as the main cause of HIV seroconversion among gay men in their late thirties.[22] The chemical "methamphetamine", in and of itself, cannot infect someone with HIV.
Washington, D.C., the nation's capital, also has the nation's highest rate of infection, at 3%. This rate is comparable to what is seen in west Africa, and is considered a severe epidemic.[23]
In Canada, nearly 60,000 people were living with HIV/AIDS in 2005.[24] The HIV-positive population continues to increase in Canada, with the greatest increases amongst aboriginal Canadians.[25] As in Western Europe, the death rate from AIDS in North America fell sharply with the introduction of combination AIDS therapies (HAART).
In the United States, young African-American women are also at high risk for HIV infection.[26] African Americans make up 10% of the population but about half of the HIV/AIDS cases nationwide.[27] This is due in part to a lack of information about AIDS and a perception that they are not vulnerable, as well as to limited access to health-care resources and a higher likelihood of sexual contact with at-risk male sexual partners.[28] There are also geographic disparities in AIDS prevalence in the United States, where it is most common in the large metropolitan areas of the east coast and California and in urban areas of the deep south.[29]
Eastern Europe and Central Asia
Main article: HIV/AIDS in Eastern Europe and Central Asia
There is also growing concern about a rapidly growing epidemic in Eastern Europe and Central Asia,
where an estimated 1.23–3.7 million people were infected in December
2011, though the adult (15–49) prevalence rate is low (1.1%). The rate
of HIV infections began to grow rapidly from the mid-1990s, due to
social and economic collapse, increased levels of intravenous drug use
and increased numbers of prostitutes. By 2010 the number of reported
cases in Russia was over 450,000 according to the World Health Organization,
up from 15,000 in 1995 and 190,000 in 2002; some estimates claim the
real number is up to eight times higher, well over 2 million. There are
predictions that the infection rate in Russia will continue to rise
quickly, since education there about AIDS is almost non-existent.[30]Ukraine and Estonia also had growing numbers of infected people, with estimates of 650,000 and 4,400 respectively in 2011. The disease is now officially epidemic in this region, which means that prevention strategies may not be able to halt and reverse its spread. Also, transmission of HIV is increasing through sexual contact and drug use among the young (<30 years). Indeed, over 84% of current AIDS cases in this region occur in non-drug-using heterosexuals less than 26 years of age.
Western Europe
| This section does not cite any references or sources. (January 2011) |
Main article: HIV/AIDS in Western Europe
In most countries of Western Europe, AIDS cases have fallen to levels
not seen since the original outbreak; many attribute this trend to
aggressive educational campaigns, screening of blood transfusions and
increased use of condoms. Also, the death rate from AIDS in Western
Europe has fallen sharply, as new AIDS therapies have proven to be an
effective (though expensive) means of suppressing HIV.In this area, the routes of transmission of HIV is diverse, including paid sex, injecting drug use, mother to child, male with male sex and heterosexual sex.[citation needed] However, many new infections in this region occur through contact with HIV-infected individuals from other regions. The adult (15–49) prevalence in this region is 0.3% with between 570,000 and 890,000 people currently infected with HIV infection. Due to the availability of antiretroviral therapy, AIDS deaths have stayed low since the lows of the late 1990s. However, in some countries, a large share of HIV infections remain undiagnosed and there is worrying evidence of antiretroviral drug resistance among some newly HIV-infected individuals in this region.
Oceania
Main articles: HIV/AIDS in Australia and HIV/AIDS in Papua New Guinea
There is a very large range of national situations regarding AIDS and
HIV in this region. This is due, in part, to the large distances
between the islands of Oceania. The wide range of development in the
region also plays an important role. The prevalence is estimated at
between 0.2% and 0.7%, with between 45,000 and 120,000 adults and
children currently infected with HIV.Papua New Guinea has one of the most serious AIDS epidemics in the region. According to UNAIDS, HIV cases in the country have been increasing at a rate of 30 percent annually since 1997, and the country's HIV prevalence rate in late 2006 was 1.3%.[31]
AIDS and society
In June 2001, the United Nations held a Special General Assembly to intensify international action to fight the HIV/AIDS epidemic as a global health issue, and to mobilize the resources needed towards this aim, labelling the situation a "global crisis".[32]Regarding the social effects of the HIV/AIDS pandemic, some sociologists suggest that AIDS has caused a "profound re-medicalization of sexuality".[33][34]
Social factors also influence HIV/AIDS. A 2003 study states that HIV and AIDS are less prevalent in Muslim populations and speculates that this may be due to the effect of several Islamic tenets, such as the avoidance of extramarital affairs and the "benefits arising from circumcision".[35]



No comments:
Post a Comment