Pus is an
exudate, typically white-yellow, yellow, or yellow-brown, formed at the site of
inflammation during
infection.
[1] An accumulation of pus in an enclosed tissue space is known as an
abscess, whereas a visible collection of pus within or beneath the
epidermis is known as a
pustule or
pimple.
Pus consists of a thin,
protein-rich fluid, known as
liquor puris, and dead
leukocytes from the body's
immune response (mostly
neutrophils). During infection,
macrophages release
cytokines which trigger neutrophils to seek the site of infection by
chemotaxis. There, the neutrophils engulf and destroy the bacteria and the bacteria resist the immune response by releasing toxins called
leukocidins.
[2] As the neutrophils die off from toxins and old age, they are
destroyed by macrophages, forming the viscous pus.
Bacteria that cause pus are called
suppurative,
pyogenic,
[2][3] or
purulent. If the agent also creates
mucus, it is called
mucopurulent. Purulent infections can be treated with an
antiseptic.
Despite normally being of a whitish-yellow hue, changes in the color
of pus can be observed under certain circumstances. Pus is sometimes
green because of the presence of
myeloperoxidase,
an intensely green antibacterial protein produced by some types of
white blood cells. Green, foul-smelling pus is found in certain
infections of
Pseudomonas aeruginosa. The greenish color is a result of the pyocyanin bacterial pigment it produces.
Amoebic abscesses of the
liver produce brownish pus, which is described as looking like "anchovy paste". Pus can also have a foul odor.
In almost all cases when there is a collection of pus in the body,
the clinician will try to create an opening for it to evacuate - this
principle has been distilled into the famous Latin aphorism "
Ubi pus, ibi evacua!"
Some common disease processes caused by pyogenic infections are
impetigo,
osteomyelitis,
septic arthritis, and
necrotizing fasciitis.
[4][not in citation given]
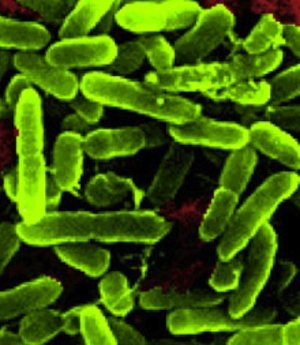
Pyogenic bacteria
A great many species of bacteria may be pyogenic. The most commonly found include:
[5][unreliable medical source?]
Exudate
From Wikipedia, the free encyclopedia
An
exudate is any
fluid that filters from the
circulatory system into
lesions or areas of
inflammation. It can apply to plants as well as animals. Its composition varies but generally includes water and the dissolved
solutes of the main circulatory fluid such as sap or blood. In the case of blood it will contain some or all
plasma proteins,
white blood cells,
platelets, and in the case of local
vascular damage:
red blood cells.
In plants, it can be a healing and defensive response to repel insect
attack, or it can be an offensive habit to repel other incompatible or
competitive plants. Organisms that feed on exudate are known as
exudativores; for example, the
Vampire Bat exhibits
hematophagy, and the
Pygmy marmoset is an
obligate gummivore[1] (primarily eats tree gum).
In humans, exudate can be a pus-like or clear fluid. When an injury
occurs, leaving skin exposed, it leaks out of the blood vessels and into
nearby tissues. The fluid is composed of serum, fibrin, and white blood
cells. Exudate may ooze from cuts or from areas of infection or
inflammation.
[2]
Inflammation
From Wikipedia, the free encyclopedia
Inflammation (
Latin,
īnflammō, "I ignite, set alight") is part of the complex biological response of
vascular tissues to harmful stimuli, such as
pathogens, damaged cells, or irritants.
[1]
The classical signs of acute inflammation are pain, heat, redness,
swelling, and loss of function. Inflammation is a protective attempt by
the organism to remove the injurious stimuli and to initiate the healing
process. Inflammation is not a synonym for
infection,
even in cases where inflammation is caused by infection. Although
infection is caused by a microorganism, inflammation is one of the
responses of the organism to the pathogen. However, inflammation is a
stereotyped response, and therefore it is considered as a mechanism of
innate immunity, as compared to
adaptive immunity, which is specific for each pathogen.
[2]
Progressive destruction of the tissue would compromise the survival
of the organism. However, chronic inflammation can also lead to a host
of diseases, such as
hay fever,
periodontitis,
atherosclerosis,
rheumatoid arthritis, and even cancer (e.g.,
gallbladder carcinoma). It is for that reason that inflammation is normally closely regulated by the body.
Inflammation can be classified as either
acute or
chronic.
Acute inflammation is the initial response of the body to harmful stimuli and is achieved by the increased movement of
plasma and
leukocytes (especially
granulocytes)
from the blood into the injured tissues. A cascade of biochemical
events propagates and matures the inflammatory response, involving the
local
vascular system, the
immune system, and various cells within the injured tissue. Prolonged inflammation, known as
chronic inflammation,
leads to a progressive shift in the type of cells present at the site
of inflammation and is characterized by simultaneous destruction and
healing of the tissue from the inflammatory process.
Staphylococcus aureus
From Wikipedia, the free encyclopedia
Staphylococcus aureus is a
bacterium that is a member of the
Firmicutes, and is frequently found in the human respiratory tract and on the skin. Although
S. aureus is not always
pathogenic, it is a common cause of skin infections (e.g.
boils), respiratory disease (e.g.
sinusitis), and
food poisoning. Disease-associated strains often promote infections by producing potent protein
toxins, and expressing cell-surface proteins that
bind and inactivate antibodies. The emergence of
antibiotic-resistant forms of pathogenic
S. aureus (e.g.
MRSA) is a worldwide problem in clinical medicine.
Staphylococcus was first identified in
Aberdeen,
Scotland (1880) by the
surgeon Sir
Alexander Ogston in
pus from a surgical abscess in a knee joint.
[1] This name was later appended to
Staphylococcus aureus
by Rosenbach who was credited by the official system of nomenclature at
the time. It is estimated that 20% of the human population are
long-term carriers of
S. aureus[2] which can be found as part of the normal
skin flora and in anterior nares of the nasal passages.
[2][3] S. aureus is the most common species of staphylococcus to cause
Staph infections and is a successful pathogen due to a combination of nasal carriage and bacterial immuno-evasive strategies.
[2][3] S. aureus can cause a range of illnesses, from minor skin
infections, such as
pimples,
impetigo,
boils (furuncles),
cellulitis folliculitis,
carbuncles,
scalded skin syndrome, and
abscesses, to life-threatening diseases such as
pneumonia,
meningitis,
osteomyelitis,
endocarditis,
toxic shock syndrome (TSS),
bacteremia, and
sepsis. Its incidence ranges from skin, soft tissue, respiratory, bone, joint, endovascular to
wound infections. It is still one of the five most common causes of
nosocomial infections
and is often the cause of postsurgical wound infections. Each year,
some 500,000 patients in American hospitals contract a staphylococcal
infection.
[4]








 Dawn Hepp shows off the wounds on her neck. (Courtesy Dawn
Dawn Hepp shows off the wounds on her neck. (Courtesy Dawn 








